Part 1 of 3 | An Honest Perspective on how health systems can navigate the risks and rewards of Medicare Advantage to drive financial and clinical success.
The Medicare Advantage crossroads
Health systems today are facing a critical decision with Medicare Advantage: take on full risk and augment their performance or risk long-term financial instability. Some organizations are fully committing, while others are walking away, citing financial pressures and operational complexities.
At the same time, Medicare Advantage payers are tightening cost controls by refining reimbursement structures, increasing administrative oversight, and enforcing stricter utilization management policies. Measures such as stricter prior authorizations, refined risk adjustment audits, and reduced provider reimbursements are reshaping how care is delivered and paid for. These shifts have increased financial pressures on providers, prompting many health systems to reevaluate their participation. With lower reimbursement rates than Traditional Medicare and mounting administrative hurdles, a growing number of health systems are exiting or scaling back their Medicare Advantage contracts.
The challenge is real for executives and providers, but so is the opportunity.
For those who approach it strategically, Medicare Advantage remains one of the strongest pathways to financial and clinical sustainability.
Here’s why:
- A growing demand – Medicare Advantage enrollment continues to rise, with over 50% of beneficiaries already enrolled and projections reaching 64% by 2034. Health systems that build effective strategies now will be positioned for long-term success as the shift toward Medicare Advantage accelerates.
- A strong foundation for performance – Health systems already employ nearly 75% of the primary care physicians who serve Medicare Advantage patients. This built-in network creates an opportunity to align provider incentives, reduce reliance on subsidies, and strengthen financial performance.
- A shift toward risk-based models – The Centers for Medicare & Medicaid Services (CMS) has set a 2030 goal to move all Traditional Medicare beneficiaries into value-based arrangements. Proactively adapting to risk-based models now allows health systems to gain greater control over patient outcomes and financial performance while staying ahead of potential regulatory and payment model changes.
By shifting the perspective from risk to opportunity, health systems can harness Medicare Advantage as a driver of financial and operational success rather than a liability.
Turning risk into reward: the path to profitability in Medicare Advantage
Full-risk arrangements are inherently “risky” and can present financial uncertainty, but when structured effectively, they can become a major driver of growth for health systems. Success depends on strategically managing the economic levers that influence revenue and expenses.
Achieving financial success in risk contracts
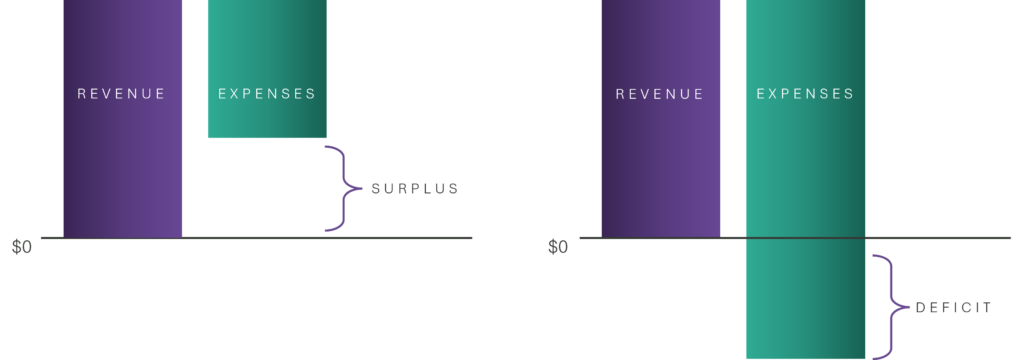
The financial outcome of a full-risk contract is determined by the balance between target revenue (payer reimbursements) and medical expenses (the cost of patient care). When managed effectively, risk contracts generate a surplus, creating a financial cushion that can be reinvested in care delivery. However, without the right cost and revenue strategies, these arrangements can lead to a deficit, exposing health systems to financial losses.
Risk surplus scenario: a well-managed model
In this scenario, the medical expenses are successfully controlled. With medical expenses contained below target revenue, the system generates a financial surplus, reinforcing sustainability and profitability in Medicare Advantage.
Risk deficit scenario: uncontrolled challenges
Here, medical expenses exceed the available revenue, leading to a financial shortfall. This often occurs when patient attribution is misaligned, risk-adjusted revenue is not maximized, or medical cost controls are not effectively implemented. Without intervention, this scenario can create significant financial risk for health systems.
In full-risk arrangements, financial success hinges on pulling the right levers:
- Patient Attribution – Ensuring accurate patient-provider alignment for effective care management.
- Revenue Optimization – Securing risk-adjusted payments that reflect patient complexity.
- Medical Expense Management – Managing care costs without compromising quality.
By strategically leveraging these factors, health systems can mitigate risk, drive profitability, and enhance patient outcomes.
Three essential levers for Medicare Advantage success
Lever #1. Accurate patient attribution
Understanding which patients are attributed to your health system is essential for optimizing care and financial outcomes. Patient attribution determines who you are responsible for and enables proactive intervention.
Key strategies for accurate attribution:
- Conduct regular patient roster reviews with PCPs to ensure alignment and data accuracy.
- Provide real-time, actionable patient-level insights to physicians to improve care planning.
- Stratify and enroll patients into high-value care management programs tailored to their specific health needs.
Lever #2. Revenue optimization through contracting and documentation
The revenue side of risk has received significant criticism over the last few years. Much of this attention is centered around organizations notorious for solely focusing on maximizing revenue through aggressive hierarchical condition category (HCC) coding. While there is reason for scrutiny, accurate risk coding remains a critical factor in aligning payment with patient complexity.
Key strategies for revenue optimization:
- Negotiate competitive premium rates with Medicare Advantage payers.
- Secure contracts with appropriate risk protections against external factors not related to providers (e.g., Star Ratings, benefit changes).
- Ensure comprehensive and accurate diagnosis documentation to align funding with actual patient risk.
Lever #3. Managing medical spend with utilization
Controlling costs does not mean restricting necessary care — it’s about making strategic decisions that improve utilization and care setting efficiency while ensuring timely, appropriate access. Traditional payer strategies like prior authorization have faced criticism, but health systems have powerful levers to control costs without compromising quality.
Key strategies for cost management:
- Build high-value specialist networks that balance cost and quality outcomes.
- Improve care setting decisions, prioritizing ambulatory care and in-office procedures where appropriate.
- Strengthen access to timely, proactive care, reducing unnecessary ER visits and readmissions.
Health systems that pull the right levers can transform financial risk into a sustainable growth strategy while delivering high-quality care.
Beyond economic promise: the value of risk
Full-risk arrangements do more than enhance financial performance — they drive greater accountability for healthcare dollars and incentivize better patient outcomes.
By prioritizing efficiency, proactive care, and patient-centered models, health systems can achieve measurable improvements in both health and financial sustainability.
Evidence consistently shows that well-executed risk-based models:
- Increase patient engagement and primary care utilization.
- Reduce avoidable hospitalizations and chronic disease complications.
- Enhance long-term financial stability by aligning costs with patient needs.
While full-risk contracts require investment and expertise, they offer a clear path to both profitability and better care delivery. Partnering with experienced organizations can help mitigate financial risks, simplify contract complexities, and accelerate success in a value-based landscape.
Health system executives and providers who are able to invest in the transition with their time, energy, and strategic collaborations with partners are well-positioned to “get risk right” and thrive in this evolving landscape. The economic promise is real, and the rewards — for patients and providers alike — make the journey worthwhile.
Coming Next: In the second installment of this three-part series, “Lining it Up: The Five Core Capabilities Needed to Perform Well with Medicare Advantage,” we explore the strategies organizations need to successfully manage and optimize full-risk Medicare Advantage performance.
“U.S. Health Expenditure as Percent of GDP 1960-2023.” Statista, Statista Inc., https://www.statista.com/statistics/184968/us-health-expenditure-as-percent-of-gdp-since-1960/. Accessed 11 Dec. 2024.
“Medicare Advantage in 2024: Enrollment Update and Key Trends.” KFF. https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2024-enrollment-update-and-key-trends/. Accessed 17 Dec. 2024.

